Sacroiliac (SI) Joint Injection
(Targeted Relief for Lower Back and Pelvic Pain)
Overview
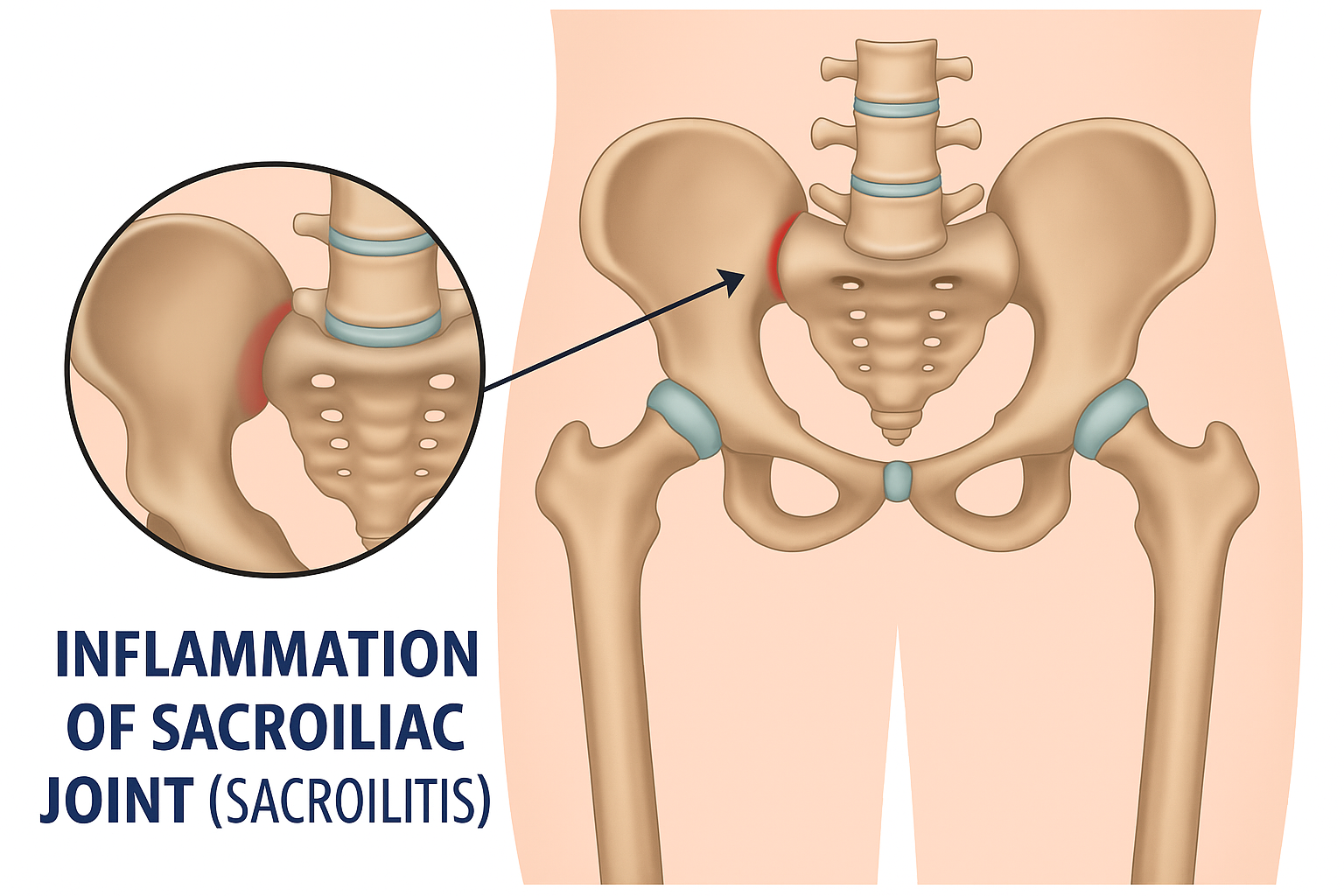
A sacroiliac (SI) joint injection is a minimally invasive procedure used to diagnose and treat pain originating from the sacroiliac joint. These joints, located where the spine meets the pelvis, can become inflamed or irritated due to injury, arthritis, pregnancy, or repetitive strain. Pain from the SI joint can mimic other spinal conditions and often causes discomfort in the lower back, buttocks, or hip region.
This injection delivers anti-inflammatory medication directly into the SI joint to reduce inflammation and provide pain relief.
Common Conditions Treated
- Sacroiliac joint dysfunction
- Degenerative sacroiliitis
- Inflammatory sacroiliitis (including ankylosing spondylitis)
- Post-traumatic or post-surgical pelvic pain
- Pain following lumbar fusion or pelvic impact injuries
What are the risks and side effects?
Risks and side effects are minimal, and serious complications are rare. We take every precaution to ensure your safety. Potential risks may include but are not limited to:
- Vasovagal response (fainting or dizziness)
- New or increased pain
- Infection
- Bleeding
- Permanent skin changes
- Allergic or unexpected drug reaction with minor or major consequences
- Unintended spinal or nerve injury
Ask your provider if you have any concerns. Your physician will review the risks in detail before the procedure to ensure you are fully informed.
Pre-Procedure Information
How Should I Prepare?
- Driver Required: We ask that you arrange for a driver to take you home after the procedure.
- Food: You may eat a light meal 1–2 hours prior to the procedure. If sedation is planned, please follow the specific sedation protocol provided by our team.
Medications:
- Continue routine medications unless directed otherwise.
-
Blood thinners, Aspirin, NSAIDs, and supplements:
- Inform us in advance if you take blood thinners (e.g., Plavix, Eliquis, Xarelto, Coumadin), NSAIDs (e.g., ibuprofen, naproxen), Aspirin, or supplements that increase bleeding risk.
- Certain medications may need to be stopped for a short period of time before the injection.
- Speak with your prescribing provider to ensure it’s safe to temporarily stop these medications.
- Our team will review your medication list and coordinate with your other providers if needed.
Notify us if:
- You have a fever, infection, or are feeling unwell.
- You have started antibiotics or had changes to your medications.
Sedation
Most procedures can be performed comfortably without sedation. However, if you have anxiety or difficulty lying flat, mild sedation may be offered at the discretion of the physician. Please discuss this with your provider in advance.
Special Instructions for Diabetic Patients
Steroid injections may raise blood sugar levels for several days.
- Please contact your primary care physician or endocrinologist prior to the procedure for management recommendations.
- Monitor your glucose closely after the injection.
- Report sustained elevations to your managing provider.
What if I am pregnant?
Most procedures can be performed comfortably without sedation. However, if you have anxiety or difficulty lying flat, mild sedation may be offered at the discretion of the physician. Please discuss this with your provider in advance.
Procedure Information
The procedure is performed using sterile technique under real-time X-ray (fluoroscopic) guidance.
What to Expect:
1 Preparation:
- You will lie face down on a procedure table
- The skin will be cleaned and numbed with a local anesthetic
2 Injection Process:
- A needle is guided into the joint space using fluoroscopy.
- Contrast dye may be used to confirm positioning.
- A corticosteroid is injected to reduce inflammation.
Monitoring:
- You will be monitored during the procedure to ensure comfort and safety.
- Most procedures last 15–30 minutes, followed by a brief recovery period on-site.
Post-Procedure Information
What to Expect After the Procedure
- Relief Timeline: : Steroids typically begin to work within 2 to 5 days, but in some cases may take up to 2 weeks.
- Activity:You may resume light activities the next day; avoid strenuous activity for 24 hours. We recommend you return to work the following day
- Soreness: Temporary soreness at the injection site is common.
- Pain tracking: Keep a log of symptoms over the next 1–2 weeks.
If successful, additional injections may be spaced out over time—typically no more than 3–4 per year in the same region.
Additional Instructions:
- Contact the office for any signs of infection, fever, or worsening pain.
- Attend follow-up as scheduled.
Schedule a Consultation
If you suffer from lower back or pelvic pain and suspect it may be related to your SI joint, Restore Spine and Pain is here to help. Contact us today to schedule an evaluation and begin your personalized treatment plan.

