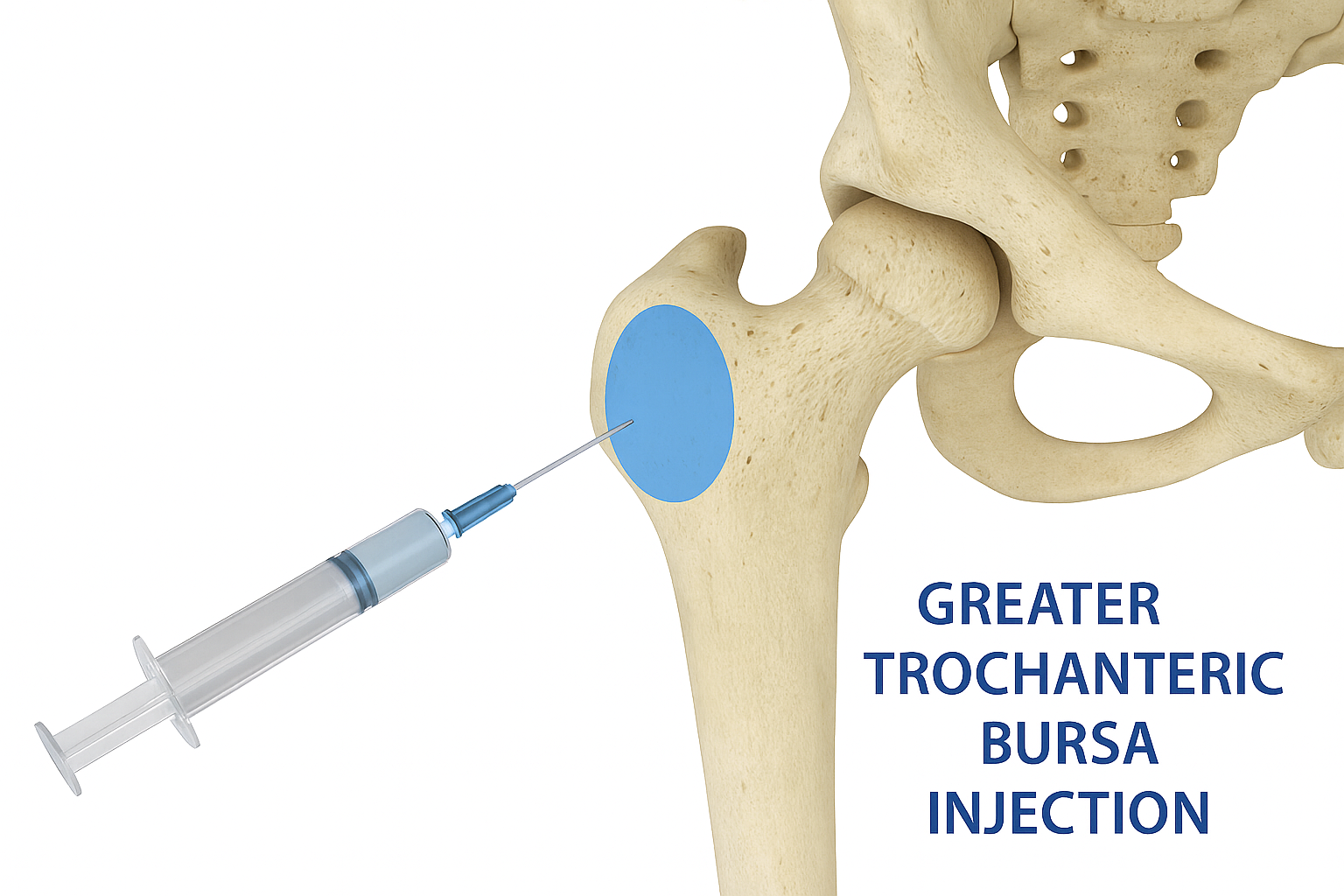
Greater Trochanteric Bursa Injection
(Targeted Relief for Hip Bursitis and Outer Hip Pain)
Overview
The greater trochanteric bursa is a fluid-filled sac located on the outside of the hip. Inflammation in this area—known as greater trochanteric bursitis—can cause significant outer hip pain, particularly when lying on the side, walking, or climbing stairs. An injection into the bursa can reduce inflammation and provide lasting relief.
At Restore Spine and Pain, this procedure is typically performed under ultrasound guidance for precision and patient comfort. In select cases, fluoroscopic (X-ray) guidance may be used.
Conditions Treated
- Greater trochanteric bursitis
- Gluteal tendinopathy or enthesopathy
- Lateral hip pain syndromes
- Post-traumatic inflammation of the hip bursa
What are the risks and side effects?
Risks and side effects are minimal, and serious complications are rare. We take every precaution to ensure your safety. Potential risks may include but are not limited to:
- Temporary flare-up of pain
- Bleeding or infection (rare)
- Vasovagal response (fainting or dizziness)
- Allergic reaction to medication
- Elevated blood sugar levels in diabetic patients
- Tendon or soft tissue injury
Ask your provider if you have any concerns. Your physician will review the risks in detail before the procedure to ensure you are fully informed.
Pre-Procedure Information
How Should I Prepare?
- Driver Required: We ask that you arrange for a driver to take you home after the procedure.
- Food: You may eat a light meal 1–2 hours prior to the procedure. If sedation is planned, please follow the specific sedation protocol provided by our team.
Medications:
- Continue routine medications unless directed otherwise.
-
Blood thinners, Aspirin, NSAIDs, and supplements:
- Inform us in advance if you take blood thinners (e.g., Plavix, Eliquis, Xarelto, Coumadin), NSAIDs (e.g., ibuprofen, naproxen), Aspirin, or supplements that increase bleeding risk.
- Certain medications may need to be stopped for a short period of time before the injection.
- Speak with your prescribing provider to ensure it’s safe to temporarily stop these medications.
- Our team will review your medication list and coordinate with your other providers if needed.
Notify us if:
- You have a fever, infection, or are feeling unwell.
- You have started antibiotics or had changes to your medications.
Special Instructions for Diabetic Patients:
Steroid injections may raise blood sugar levels for several days
- Please contact your primary care physician or endocrinologist prior to the procedure for management recommendations.
- Monitor your glucose closely after the injection.
- Report sustained elevations to your managing provider.
What if I am pregnant?
There are serious potential risks to an unborn fetus from imaging used during this procedure (e.g., X-ray/fluoroscopy). If there is any chance you may be pregnant, please notify our team immediately and postpone the injection until pregnancy is ruled out.
Procedure Information
The procedure is performed using sterile technique under real-time image guidance
What to Expect:
1 Preparation:
- You will be positioned accordingly.
- The skin will be cleaned and numbed with a local anesthetic.
2 Injection Process:
- A needle is guided into the joint space using fluoroscopy.
- Contrast dye may be used to confirm positioning.
- A mixture of local anesthetic and corticosteroid is injected to reduce inflammation.
3 Monitoring:
- You will be monitored during the procedure to ensure comfort and safety.
- Most procedures last 15–30 minutes, followed by a brief recovery period on-site.
Post-Procedure Information
What to Expect After the Procedure
- Relief Timeline: : Steroids typically begin to work within 2 to 5 days, but in some cases may take up to 2 weeks.
- Activity:You may resume light activities the next day; avoid strenuous activity for 24 hours. We recommend you return to work the following day
- Soreness: Temporary soreness at the injection site is common.
- Pain tracking: Keep a log of symptoms over the next 1–2 weeks.
If successful, additional injections may be spaced out over time—typically no more than 3–4 per year in the same region.
Additional Instructions:
- Contact the office for any signs of infection, fever, or worsening pain.
- Attend follow-up as scheduled.
Schedule a Consultation
If you are experiencing outer hip pain or discomfort due to bursitis or tendon inflammation, contact Restore Spine and Pain for a thorough evaluation and image-guided treatment options.

